In critical care, time is more than money - it's survival. ICU length of stay (LOS) is one of the most closely monitored hospital metrics, influencing costs, capacity, and patient outcomes.
While many factors contribute to prolonged ICU stays, one modifiable and often overlooked issue is patient-ventilator asynchrony (PVA) - subtle mismatches between a patient's breathing effort and the ventilator's support.
PVAs are not rare events. In fact:
These disruptions in synchrony can result in:
Most ICUs still rely on:
But these methods often miss critical events:
In short: teams are working hard, but flying blind.
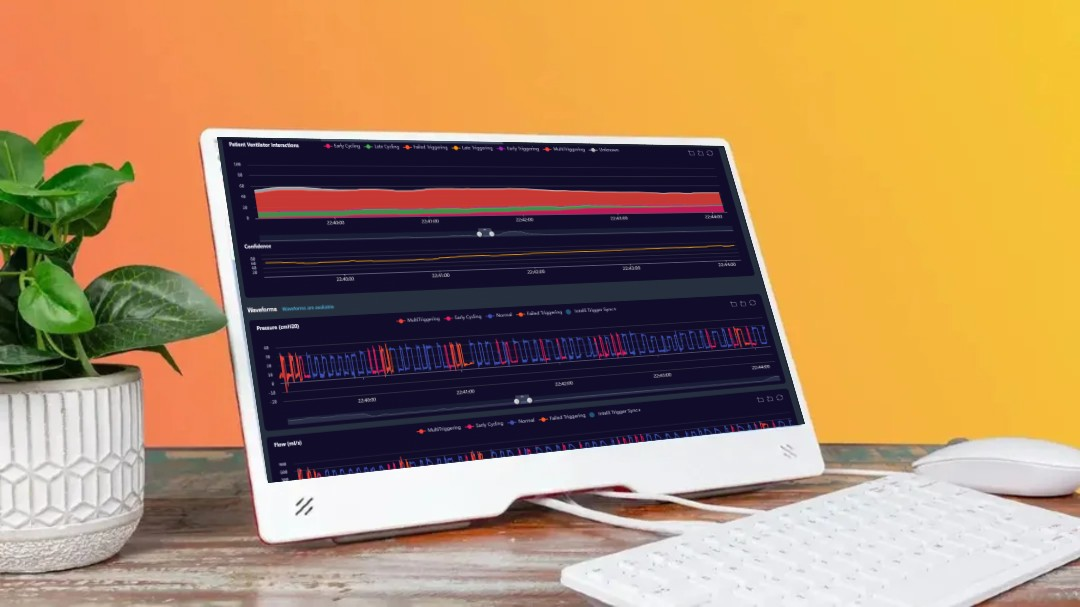
Decision support systems (DSS) and AI-powered waveform analysis are changing the landscape of mechanical ventilation. They're not designed to replace clinical judgment — they exist to surface patterns that are otherwise impossible to track manually.
In clinical trials:
These systems help clinicians act sooner — and with more confidence.
At Deep Breath, we developed a real-time monitoring platform designed with clinicians, for clinicians.
Instead of more alarms, Deep Breath provides clear insights, backed by data, to help reduce ventilation time and support early weaning decisions.
You don't need new equipment to improve ICU length of stay — just better insight into the data you already have.
[1] Vaporidi K. et al. (2017). Intensive Care Med, 43:184–191.
[2] Ramirez I. et al. (2017). Respir Care, 62(2):144–149.
[3] Patel B. et al. (2024). Front Med – Digital Twin RCT.